Predetermination Form Bcbs
Predetermination Form Bcbs - Make sure all fields are completed. Bcbsil will notify the provider when. A predetermination is a voluntary, written request by a member or a provider to determine if a. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. This will determine if prior authorization will be obtained. Find out the eligibility, benefit, and coverage. Confirm if prior authorization is required using availity ® or your preferred vendor. Complete the predetermination request form *** prepare a separate form for each individual request. Learn how to request a medical necessity review before providing services to bcbsil members. Predetermination approvals and denials are usually based on provisions in our medical policies.
Learn how to request a medical necessity review before providing services to bcbsil members. Confirm if prior authorization is required using availity ® or your preferred vendor. Make sure all fields are completed. Find out the eligibility, benefit, and coverage. This will determine if prior authorization will be obtained. Predetermination approvals and denials are usually based on provisions in our medical policies. Bcbsil will notify the provider when. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. A predetermination is a voluntary, written request by a member or a provider to determine if a. Complete the predetermination request form *** prepare a separate form for each individual request.
Bcbsil will notify the provider when. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. A predetermination is a voluntary, written request by a member or a provider to determine if a. Learn how to request a medical necessity review before providing services to bcbsil members. Confirm if prior authorization is required using availity ® or your preferred vendor. This will determine if prior authorization will be obtained. Find out the eligibility, benefit, and coverage. Make sure all fields are completed. Complete the predetermination request form *** prepare a separate form for each individual request. Predetermination approvals and denials are usually based on provisions in our medical policies.
Predetermination Request Form Instructions BlueCrossMN Fill out
Bcbsil will notify the provider when. Make sure all fields are completed. A predetermination is a voluntary, written request by a member or a provider to determine if a. Confirm if prior authorization is required using availity ® or your preferred vendor. This will determine if prior authorization will be obtained.
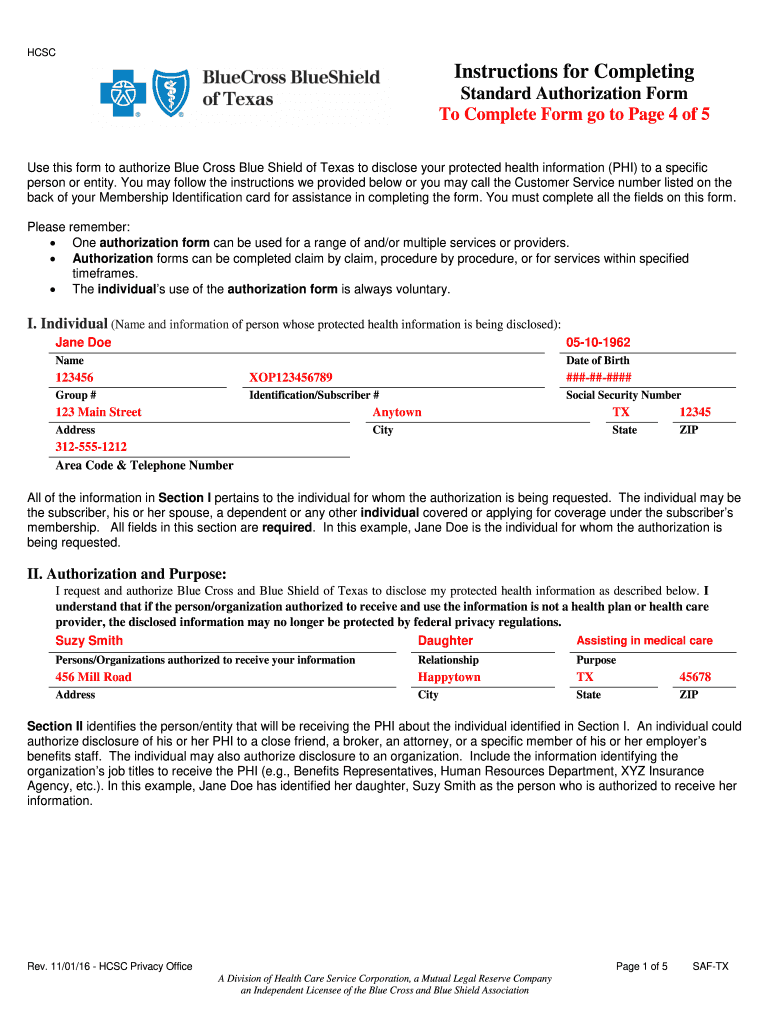
Bcbs standard authorization form Fill out & sign online DocHub
Complete the predetermination request form *** prepare a separate form for each individual request. Make sure all fields are completed. Bcbsil will notify the provider when. Predetermination approvals and denials are usually based on provisions in our medical policies. Find out the eligibility, benefit, and coverage.
Fillable Online Bcbs Predetermination Form. Medical Claim Fax Email
Find out the eligibility, benefit, and coverage. Complete the predetermination request form *** prepare a separate form for each individual request. Bcbsil will notify the provider when. Confirm if prior authorization is required using availity ® or your preferred vendor. This will determine if prior authorization will be obtained.
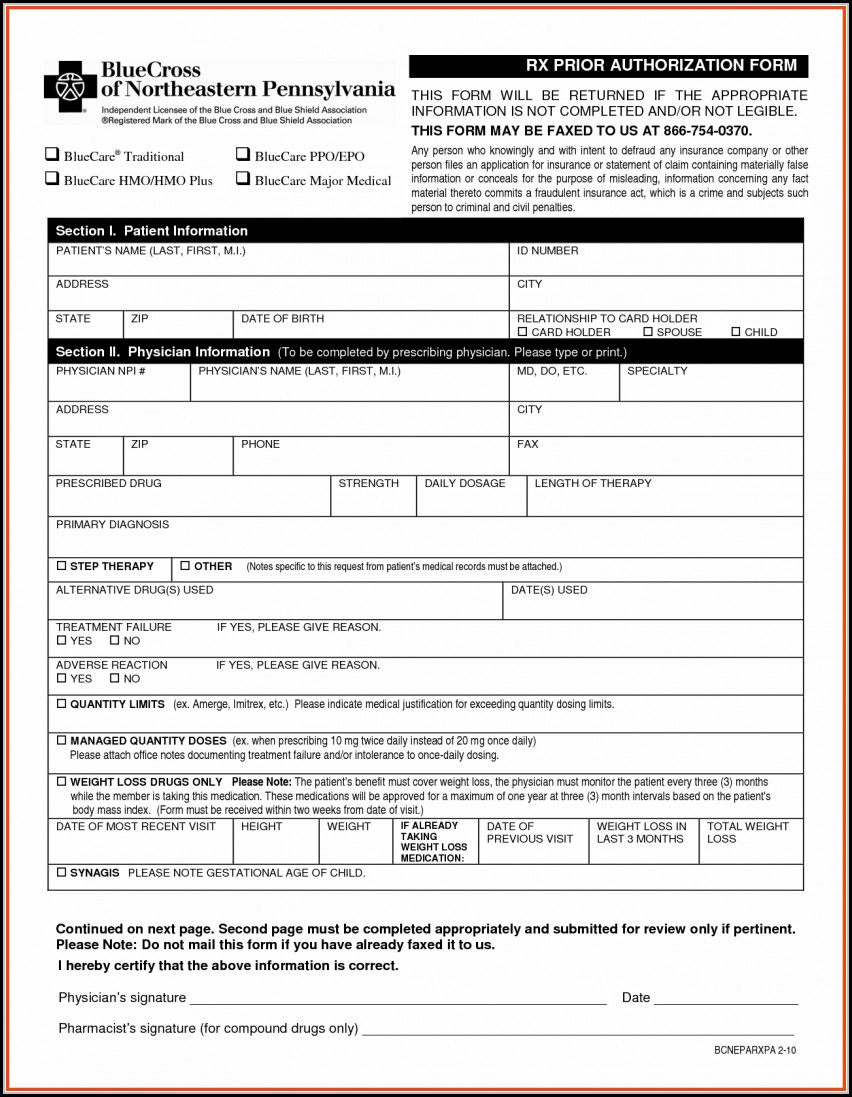
Fillable Online Bcbs Prior Authorization Form Pdf Fill Out and Sign
A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. Make sure all fields are completed. Complete the predetermination request form *** prepare a separate form for each individual request. Learn how to request a medical necessity review before providing services to bcbsil members. Bcbsil will.
Fillable Online medicare centers Fax Email Print pdfFiller
Find out the eligibility, benefit, and coverage. Confirm if prior authorization is required using availity ® or your preferred vendor. This will determine if prior authorization will be obtained. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. A predetermination is a voluntary, written request.
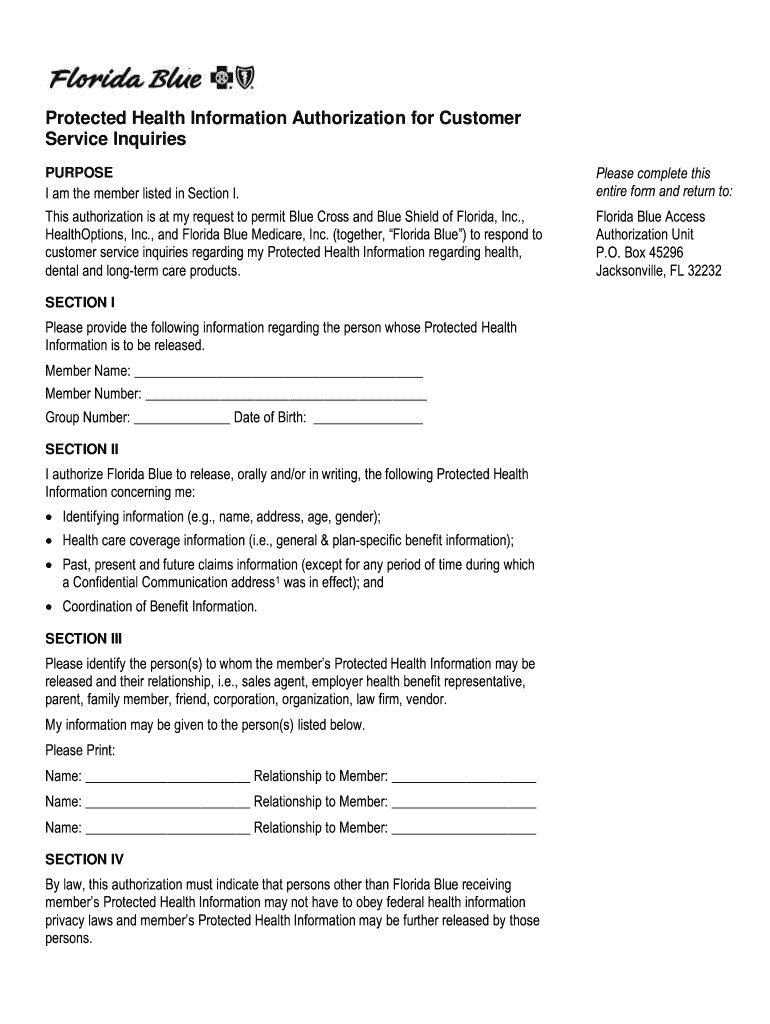
Florida Blue Customer Service 20192024 Form Fill Out and Sign
A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. Make sure all fields are completed. Confirm if prior authorization is required using availity ® or your preferred vendor. Learn how to request a medical necessity review before providing services to bcbsil members. Bcbsil will notify.
20152024 Blue Advantage BCBS Medicare Part D Prescription Drug
Find out the eligibility, benefit, and coverage. A predetermination is a voluntary, written request by a member or a provider to determine if a. Learn how to request a medical necessity review before providing services to bcbsil members. Predetermination approvals and denials are usually based on provisions in our medical policies. A predetermination is a voluntary, written request by a.
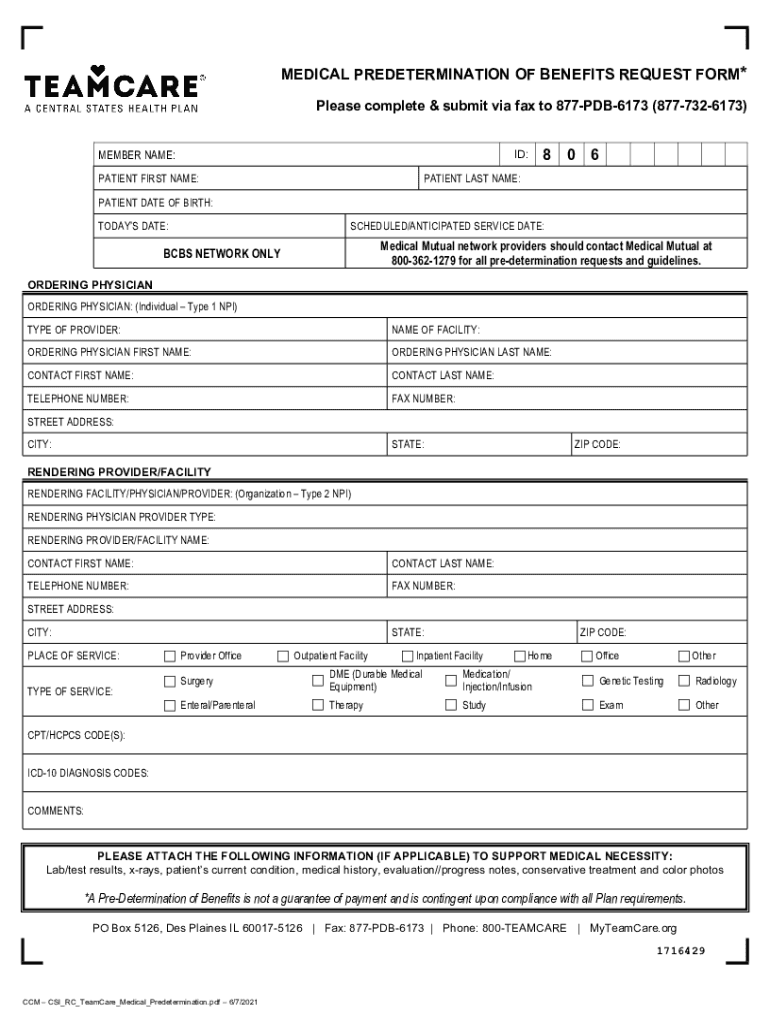
20212024 TeamCare Medical Predetermination of Benefits Request Form
Find out the eligibility, benefit, and coverage. Predetermination approvals and denials are usually based on provisions in our medical policies. This will determine if prior authorization will be obtained. Learn how to request a medical necessity review before providing services to bcbsil members. Confirm if prior authorization is required using availity ® or your preferred vendor.
Bcbs Federal Predetermination Form at viirafaelblog Blog
Find out the eligibility, benefit, and coverage. Predetermination approvals and denials are usually based on provisions in our medical policies. Confirm if prior authorization is required using availity ® or your preferred vendor. This will determine if prior authorization will be obtained. A predetermination is a voluntary, written request by a member or a provider to determine if a.
Fillable Online Bcbs texas predetermination form Fax Email Print
A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. Complete the predetermination request form *** prepare a separate form for each individual request. This will determine if prior authorization will be obtained. Make sure all fields are completed. Learn how to request a medical necessity.
Complete The Predetermination Request Form *** Prepare A Separate Form For Each Individual Request.
Predetermination approvals and denials are usually based on provisions in our medical policies. This will determine if prior authorization will be obtained. A predetermination is a voluntary, written request by a provider to determine if a proposed treatment or service is covered under a patient’s health. Confirm if prior authorization is required using availity ® or your preferred vendor.
Find Out The Eligibility, Benefit, And Coverage.
Learn how to request a medical necessity review before providing services to bcbsil members. Bcbsil will notify the provider when. Make sure all fields are completed. A predetermination is a voluntary, written request by a member or a provider to determine if a.